- Introduction
- Definition of External Respiration
- Importance of External Respiration
- Introduction
Welcome to the fascinating world of external respiration, the fundamental process that keeps us alive by supplying our bodies with the essential oxygen we need to thrive. In this article, we’ll embark on a journey to uncover the secrets of external respiration, from its definition to its profound importance in our daily lives.
- Definition of External Respiration
External respiration, often referred to as breathing, is the remarkable process by which our bodies exchange gases with the surrounding environment. It involves inhaling fresh oxygen-rich air and exhaling carbon dioxide, a waste product produced by our cells. This process primarily occurs in our lungs and is crucial for our survival.
- Importance of External Respiration
Why is external respiration so vital? Let’s break it down in simple terms:
Oxygen is Life: Oxygen is like the superhero of gases; it’s essential for the functioning of every cell in our body. Without a steady supply of oxygen, our cells wouldn’t be able to generate energy, and our bodies would come to a grinding halt.
Eliminating Waste: Just as we need oxygen, our bodies produce carbon dioxide as a waste product when we use oxygen. If we don’t get rid of this carbon dioxide, it can build up in our bloodstream and become harmful. External respiration allows us to expel this waste gas safely.
Maintaining Balance: External respiration also plays a crucial role in maintaining the balance of chemicals in our body, particularly the pH level. When we breathe, we help keep the level of acidity in our blood in check, which is vital for our overall health.
Adaptation: External respiration isn’t just about day-to-day survival. Our bodies can adapt to different conditions, like high altitudes or underwater environments, by adjusting the way we breathe. This adaptability ensures we can function effectively even in challenging situations.
In essence, external respiration is the cornerstone of life itself. It’s the process that provides our cells with the oxygen they crave and keeps our internal environment in harmony. Without it, our bodies would struggle to function, and life as we know it would cease to exist.
So, let’s dive deeper into the inner workings of this incredible process and explore how our bodies master the art of breathing.
- Anatomy of the Respiratory System
- Nasal Cavity and Pharynx
- Larynx and Trachea
- Bronchial Tree
- Alveoli
- Nasal Cavity and Pharynx
Our journey into the world of breathing begins at the very entrance of our respiratory system: the nasal cavity and the pharynx.
Nasal Cavity: This is the space inside our nose. It’s not just for smelling; it’s also a clever air conditioner. As air enters, it’s warmed, moistened, and cleaned by tiny hairs called cilia and mucus. This ensures that the air we breathe in is comfy and ready for its journey deeper into our lungs.
Pharynx: Moving southward, we reach the pharynx, a sort of crossroads where the path to our lungs intersects with the path to our stomach. The pharynx helps direct the air down the right path, allowing us to breathe without choking on our food.
- Larynx and Trachea
Continuing our exploration, we encounter the larynx and trachea. These structures play a pivotal role in our ability to speak and, more importantly, breathe smoothly.
Larynx (Voice Box): The larynx, affectionately known as the voice box, houses our vocal cords. When we speak or sing, air from our lungs passes over these cords, causing them to vibrate and create sound. It’s like our personal musical instrument!
Trachea (Windpipe): Think of the trachea as the highway for air. It’s a sturdy tube that ensures air reaches our lungs. To protect this vital route, it’s lined with rings of cartilage, much like a flexible tunnel, preventing it from collapsing while we breathe.
- Bronchial Tree
As we venture deeper, we arrive at the bronchial tree, a branching network that resembles an upside-down tree. This complex structure plays a crucial role in distributing air efficiently.
Bronchi: The trachea divides into two bronchi, one leading to each lung. These bronchi further branch into smaller tubes called bronchioles. They act like the branches of our respiratory tree, ensuring that air reaches every corner of our lungs.
- Alveoli
Our exploration concludes with the alveoli, tiny air sacs at the end of the bronchioles. These microscopic sacs are where the real magic of external respiration happens.
Gas Exchange: Alveoli are like the exchange counters for oxygen and carbon dioxide. They are surrounded by tiny blood vessels called capillaries. Here, oxygen from the inhaled air crosses into our blood, while carbon dioxide from our blood enters the alveoli to be expelled when we exhale. This exchange is vital for our body to receive oxygen and get rid of waste gases.
The anatomy of the respiratory system is nothing short of remarkable. Each part has a unique function, ensuring that the air we breathe is filtered, conditioned, and delivered to the tiny alveoli where the essential exchange of gases takes place. It’s a beautifully designed system that allows us to breathe effortlessly, day in and day out.
Now that we’ve navigated the airways, we’ll delve deeper into the process of external respiration, uncovering how all these components work harmoniously to keep us alive and well.
III. The Process of External Respiration
- Ventilation
- Inspiration
- Expiration
- Gas Exchange
- Diffusion of Oxygen
- Diffusion of Carbon Dioxide
- Role of the Respiratory Muscles
- Respiratory Volumes and Capacities
III. The Process of External Respiration: Breathing Life In and Out
Now that we’ve explored the fascinating anatomy of the respiratory system, it’s time to dive into the nitty-gritty of how external respiration works. This process is nothing short of miraculous, as it allows us to bring life-sustaining oxygen into our bodies and remove the waste carbon dioxide. Let’s break it down step by step.
- Ventilation
- Inspiration
Inspiration, the scientific term for inhaling, is the first step in the respiratory process. It’s like taking a refreshing sip of air. Here’s how it happens:
Diaphragm and Intercostal Muscles: When you decide to take a breath, your diaphragm (a large muscle beneath your lungs) contracts and flattens, while the intercostal muscles (between your ribs) lift your ribcage. This expansion increases the volume in your chest cavity, creating a partial vacuum.
Air Rushes In: Nature abhors a vacuum, and so does your body. Air from the outside rushes in through your nose and mouth, following the path we learned about earlier. It travels down the trachea, into the bronchi, and eventually reaches the alveoli, where the real magic happens.
- Expiration
Expiration, the fancy word for exhaling, is the next part of the respiratory process. It’s like a relaxing sigh, but it’s much more critical to our survival than just letting out a breath.
Relaxation Time: After inhaling, your diaphragm and intercostal muscles relax. This reduces the chest cavity’s volume, causing pressure inside your lungs to increase.
Air Gets Pushed Out: High-pressure air inside your lungs now wants to escape. It follows the reverse route, traveling from the alveoli up through the bronchi, trachea, and out through your nose or mouth. And there you have it, a simple exhale!
- Gas Exchange
Now, let’s delve into the remarkable gas exchange that occurs in the alveoli.
- Diffusion of Oxygen
Oxygen-Hungry Blood: Deoxygenated blood, which has just returned from various parts of your body, arrives at the alveoli. It’s thirsty for oxygen.
Oxygen-Rich Air: The inhaled air in the alveoli is rich in oxygen. Oxygen molecules happily jump across the thin walls of the alveoli and into the surrounding capillaries (tiny blood vessels). This is where oxygen and blood become fast friends.
- Diffusion of Carbon Dioxide
Carbon Dioxide Departure: In contrast, carbon dioxide in the oxygen-poor blood diffuses out of the capillaries and into the alveoli. It’s a one-way ticket out of your body.
- Role of the Respiratory Muscles
All of these actions—inspiration and expiration—aren’t random. They’re carefully orchestrated by your respiratory muscles, especially the diaphragm and intercostal muscles. These muscles contract and relax in perfect harmony, creating the changes in chest volume that drive the ventilation process.
- Respiratory Volumes and Capacities
We also have a way to measure the efficiency of this process. Respiratory volumes and capacities are like the statistics of your breathing.
Tidal Volume: This is the amount of air you inhale and exhale during a regular breath. It’s like a single sip of air.
Inspiratory Reserve Volume: Ever need to take a really deep breath? That’s your inspiratory reserve volume in action. It’s the extra air you can inhale beyond your regular tidal volume.
Expiratory Reserve Volume: Similarly, if you force out more air than usual, that’s your expiratory reserve volume at work. It’s the extra push you can give during an exhale.
Vital Capacity: This is the total amount of air you can move in and out of your lungs with the deepest possible breaths. It’s like your lung’s maximum capacity.
Understanding these respiratory volumes and capacities helps doctors diagnose lung conditions and assess overall lung health.
So, there you have it! The process of external respiration, from taking a simple breath to the intricate gas exchange in the alveoli, is a symphony of bodily functions working together seamlessly to keep you alive and well. It’s truly a marvel of nature. Next, we’ll explore the factors that influence external respiration and the mechanisms that keep it finely tuned.
- Factors Affecting External Respiration
- Partial Pressure of Gases
- Surface Area of the Alveoli
- Thickness of the Respiratory Membrane
- Lung Diseases and Disorders
- Factors Affecting External Respiration: The Breath’s Balancing Act
As we continue our journey through the world of external respiration, we come across the factors that influence this life-sustaining process. It’s like examining the gears that keep the respiratory system ticking smoothly. Let’s dive right in and explore these crucial factors.
- Partial Pressure of Gases
To understand the role of partial pressure, imagine the air we breathe as a big bowl of soup, but instead of flavors, it’s filled with gases like oxygen and carbon dioxide. Each gas in this soup exerts its own pressure, known as partial pressure, just like different ingredients in a soup contribute to its taste.
Oxygen Pressure: The partial pressure of oxygen (abbreviated as PO2) is crucial for external respiration. It determines how much oxygen can dissolve in your blood and get delivered to your cells. At high altitudes, where the air is thinner, PO2 is lower, making it harder for your body to get enough oxygen.
Carbon Dioxide Pressure: Similarly, the partial pressure of carbon dioxide (abbreviated as PCO2) affects how effectively you can get rid of this waste gas. If PCO2 levels rise too much, it can lead to a condition known as respiratory acidosis, where your blood becomes too acidic.
Balancing these pressures is essential for external respiration to function optimally. Thankfully, your body has mechanisms in place to regulate them, ensuring you get the right amount of oxygen and expel carbon dioxide efficiently.
- Surface Area of the Alveoli
Picture the alveoli, those tiny air sacs in your lungs, as a bustling marketplace. The more stalls (surface area) you have, the more trade (gas exchange) can happen. Here’s why this matters:
Efficient Exchange: To facilitate gas exchange, you need a vast surface area in your lungs. This is precisely what the countless alveoli provide. They create a massive area where oxygen can hop into your bloodstream and carbon dioxide can hop out.
Diseases and Surface Area: Some lung diseases, like emphysema, can damage the alveoli and reduce their surface area. This diminishes the efficiency of external respiration, making it harder for your body to get the oxygen it needs.
- Thickness of the Respiratory Membrane
The respiratory membrane is like the delicate parchment paper that separates your alveoli from your blood vessels. It’s incredibly thin, about one-thousandth the thickness of a human hair. This thinness is essential for efficient gas exchange.
Gas Crossing: The thin respiratory membrane allows gases to diffuse (move) quickly between the alveoli and your blood. If the membrane thickens due to inflammation or disease, it becomes a roadblock, slowing down gas exchange.
Efficiency Matters: Any hindrance to this thin membrane’s function can disrupt external respiration, affecting the balance of oxygen and carbon dioxide in your body.
- Lung Diseases and Disorders
Unfortunately, not all lungs are in perfect working order. Lung diseases and disorders can throw a wrench into the gears of external respiration. Here are a few examples:
Chronic Obstructive Pulmonary Disease (COPD): Conditions like chronic bronchitis and emphysema, which fall under the COPD umbrella, can obstruct airways and damage lung tissues. This makes it harder to breathe and reduces the efficiency of external respiration.
Asthma: Asthma narrows airways, making it challenging to move air in and out. During asthma attacks, external respiration can become severely compromised.
Pneumonia: This lung infection can fill the alveoli with pus and other fluids, reducing the surface area available for gas exchange.
Understanding these factors affecting external respiration is crucial for maintaining good respiratory health. Our bodies are designed to adapt and compensate, but keeping our respiratory system in top shape through a healthy lifestyle and regular check-ups is the best way to ensure smooth and efficient breathing.
As we move forward in our exploration, we’ll delve into how our bodies regulate external respiration, maintaining the delicate balance of gases in our blood to keep us alive and well.
- Regulation of External Respiration
- The Role of Chemoreceptors
- Control of Breathing
- Central Respiratory Centers
- Peripheral Chemoreceptors
- Influence of Blood pH and Carbon Dioxide Levels
- Regulation of External Respiration: The Breath’s Conductors
Now that we’ve unraveled the factors affecting external respiration, let’s delve into the remarkable mechanisms that regulate this essential process. Think of these mechanisms as the maestros of an orchestra, guiding the symphony of your breath.
- The Role of Chemoreceptors
Chemoreceptors are the body’s sensors that keep a vigilant eye on the chemical composition of your blood and decide when it’s time to adjust your breathing.
Oxygen Sensors: While oxygen is crucial, your body doesn’t primarily regulate breathing based on oxygen levels. Surprisingly, it’s more concerned with carbon dioxide and pH.
Carbon Dioxide Detectors: Specialized chemoreceptors in your brain and arteries monitor carbon dioxide (CO2) levels. If CO2 levels rise, it’s a sign that your body isn’t getting rid of enough waste gas. This triggers increased ventilation (breathing) to expel excess CO2.
- Control of Breathing
Breathing isn’t something you have to think about consciously; it’s an automatic process controlled by specific centers in your brain and feedback from chemoreceptors.
- Central Respiratory Centers
Medulla Oblongata: This part of your brain, located at the base of the brainstem, houses the primary respiratory centers. They set the basic rhythm of your breathing.
Pons: Just above the medulla, the pons fine-tunes your breathing rhythm. It helps adjust the rate and depth of your breaths, depending on your body’s needs.
- Peripheral Chemoreceptors
Carotid Bodies and Aortic Bodies: These are like the backup singers in the respiratory choir. Located in your carotid arteries and aorta, they continuously monitor blood chemistry. When they detect changes, they send signals to the central respiratory centers to adjust your breathing accordingly.
- Influence of Blood pH and Carbon Dioxide Levels
Your blood’s pH level (a measure of acidity or alkalinity) is tightly regulated, and your breathing plays a significant role in maintaining this balance.
pH Balance: If your blood becomes too acidic due to factors like excessive CO2 levels, your body increases ventilation to remove excess CO2 and restore a healthy pH balance.
CO2 and Breathing: When CO2 levels rise, your body responds by increasing the rate and depth of your breaths. This helps eliminate excess CO2 and prevents a drop in blood pH.
These control mechanisms ensure that external respiration keeps your blood’s pH within a narrow, healthy range. They also guarantee that your body gets the oxygen it needs while efficiently removing waste carbon dioxide.
So, next time you take a deep breath without even thinking about it, remember that there’s a remarkable orchestra of chemoreceptors, brain centers, and feedback loops working diligently to keep your breathing in harmony. Understanding these regulatory mechanisms helps us appreciate the beauty of our body’s intricate design and the importance of maintaining our respiratory health.
As we continue our journey through the world of external respiration, we’ll explore how gases are transported in the blood and how this process ensures every cell in your body gets the oxygen it needs to thrive.
- Gas Transport in the Blood
- Hemoglobin and Oxygen Binding
- Oxygen-Hemoglobin Dissociation Curve
- Carbon Dioxide Transport
- Bicarbonate Ion Formation
- Carbaminohemoglobin
- Gas Transport in the Blood: The Vital Highway
Now that we’ve understood the intricate dance of breathing and the factors that regulate it, let’s explore how our body ensures that the precious oxygen we inhale reaches every nook and cranny, and how it efficiently clears away the waste carbon dioxide. It’s like a well-coordinated highway system within our bloodstream.
- Hemoglobin and Oxygen Binding
The MVP (Most Valuable Player) in this transport system is hemoglobin, a protein found in red blood cells. Hemoglobin has a special talent: it can bind to oxygen molecules like a magnet.
Oxygen Pickup: As blood flows through your lungs, hemoglobin grabs onto oxygen from the alveoli. Each hemoglobin molecule can carry up to four oxygen molecules, making it incredibly efficient at loading up on oxygen.
Oxygen Delivery: Hemoglobin becomes the delivery truck for oxygen. It cruises through your bloodstream, releasing oxygen to the needy cells throughout your body. This is how oxygen reaches your muscles, organs, and every other tissue that needs it.
- Oxygen-Hemoglobin Dissociation Curve
The relationship between hemoglobin and oxygen isn’t static; it depends on various factors, like the concentration of oxygen in your blood and the needs of your body. The oxygen-hemoglobin dissociation curve illustrates this relationship.
Oxygen Affinity: The curve shows how readily hemoglobin binds to oxygen. When oxygen levels are high (like in your lungs), hemoglobin eagerly grabs oxygen. When oxygen levels drop (like in your body tissues), hemoglobin releases oxygen more readily, ensuring it reaches where it’s needed most.
Bohr Effect: The curve also demonstrates the Bohr effect, which reveals how pH and carbon dioxide levels influence the binding and release of oxygen. When tissues produce more CO2 (which makes the blood slightly acidic), hemoglobin releases oxygen more readily to help counteract the acidity.
- Carbon Dioxide Transport
While oxygen is essential, we also need a system to transport and remove carbon dioxide, a waste product of energy production in our cells.
- Bicarbonate Ion Formation
CO2 Dissolved: Some carbon dioxide dissolves directly in the blood plasma, but this isn’t very efficient.
Bicarbonate Formation: The majority of CO2 is converted into bicarbonate ions (HCO3-) in your red blood cells. This process is catalyzed by an enzyme called carbonic anhydrase. Bicarbonate ions are stable and can safely travel in your bloodstream.
- Carbaminohemoglobin
CO2 Binding: Some CO2 binds directly to hemoglobin, forming a compound called carbaminohemoglobin. This allows for the safe transportation of CO2 back to the lungs.
Unloading in the Lungs: In the lungs, where CO2 levels are lower, bicarbonate ions are converted back into CO2, which can be exhaled. Similarly, carbaminohemoglobin releases CO2, allowing it to be expelled when you breathe out.
This elegant system ensures that carbon dioxide is effectively transported from your body’s cells to your lungs, where it’s expelled when you exhale. Simultaneously, oxygen-rich blood is carried to every corner of your body by hemoglobin, ensuring your cells receive the oxygen they need to function optimally.
The orchestration of these processes is a testament to the intricacy of the human body. Every breath you take plays a vital role in this dynamic system, ensuring your cells receive the oxygen they crave and that waste carbon dioxide is efficiently removed. It’s a true marvel of biology, keeping you alive and well day in and day out.
As we conclude our journey through external respiration, we’ll explore the interplay between external and internal respiration and how your cells use the oxygen delivered to them to produce the energy that fuels your daily activities.
VII. Clinical Implications and Pathologies
- Respiratory Disorders
- Chronic Obstructive Pulmonary Disease (COPD)
- Asthma
- Pneumonia
- Respiratory Assessment and Diagnosis
- Treatment Options
VII. Clinical Implications and Pathologies: Navigating the Breath’s Challenges
As we venture deeper into the world of external respiration, it’s essential to explore the bumps in the road that can disrupt this harmonious process. We’ll delve into common respiratory disorders, how experts assess and diagnose them, and the array of treatment options available.
- Respiratory Disorders
- Chronic Obstructive Pulmonary Disease (COPD)
COPD is like an unwelcome guest that overstays its welcome in your lungs. It’s an umbrella term for conditions like chronic bronchitis and emphysema, which obstruct airways and make it harder to breathe.
Symptoms: COPD typically brings symptoms like persistent coughing, increased mucus production, shortness of breath, and wheezing.
Causes: Smoking is a major contributor to COPD, but long-term exposure to lung irritants like air pollution and dust can also lead to this condition.
Management: While there’s no cure for COPD, management includes lifestyle changes (like quitting smoking), medications to open airways, and pulmonary rehabilitation programs to improve lung function.
- Asthma
Asthma is like an unpredictable houseguest who shows up unannounced, causing sudden breathing difficulties.
Symptoms: Asthma triggers episodes of wheezing, coughing, chest tightness, and shortness of breath.
Triggers: Various triggers, from allergens to cold air and stress, can set off asthma attacks.
Treatment: Asthma can often be controlled with medications like bronchodilators and inhaled corticosteroids. Lifestyle changes and asthma action plans help individuals manage the condition effectively.
- Pneumonia
Pneumonia is like an unwanted visitor that brings fever, chills, and a nasty cough.
Symptoms: Pneumonia causes inflammation in the air sacs of the lungs, leading to symptoms like high fever, chest pain, productive cough, and fatigue.
Causes: Bacterial, viral, or fungal infections can trigger pneumonia. It can also develop as a complication of other respiratory illnesses.
Treatment: Treatment depends on the cause of pneumonia but typically involves antibiotics for bacterial infections, antiviral medications for viruses, and supportive care like rest and hydration.
- Respiratory Assessment and Diagnosis
When respiratory symptoms strike, it’s crucial to assess and diagnose the issue accurately.
Physical Examination: Healthcare providers may listen to your chest with a stethoscope to detect abnormal breath sounds and examine your overall respiratory health.
Pulmonary Function Tests: These tests measure lung function and capacity, helping diagnose conditions like asthma and COPD.
Imaging: X-rays and CT scans can provide detailed images of the lungs to identify infections, tumors, or structural abnormalities.
Blood Tests: Blood tests can reveal signs of infection or inflammation, aiding in the diagnosis of respiratory illnesses.
- Treatment Options
Treatment options for respiratory disorders vary depending on the condition and its severity.
Medications: Depending on the diagnosis, medications like bronchodilators, anti-inflammatory drugs, and antibiotics may be prescribed.
Lifestyle Changes: Quitting smoking, managing allergies, and avoiding triggers are often essential components of respiratory disorder management.
Pulmonary Rehabilitation: These programs offer exercise, education, and support to improve lung function and overall quality of life.
Oxygen Therapy: For severe respiratory conditions, supplemental oxygen may be necessary to maintain healthy oxygen levels in the blood.
Surgery: In some cases, surgery may be required to remove tumors, repair damaged lung tissue, or treat severe lung diseases.
Understanding these clinical implications and pathologies empowers individuals to recognize and manage respiratory issues effectively. If you or a loved one experiences persistent respiratory symptoms, seeking medical evaluation is essential for early diagnosis and appropriate treatment. In many cases, prompt intervention can significantly improve the outlook for individuals with respiratory disorders, allowing them to breathe easier and live healthier lives.
VIII. Interplay with Internal Respiration
- Connection to Cellular Respiration
- Oxygen Delivery to Tissues
- Removal of Cellular Waste
VIII. Interplay with Internal Respiration: The Breath Within
As we continue our exploration of the breath’s wonders, it’s time to unravel the profound connection between external and internal respiration. These two processes are like partners in a well-choreographed dance, ensuring that every cell in your body gets the oxygen it craves and efficiently removes the waste it produces.
- Connection to Cellular Respiration
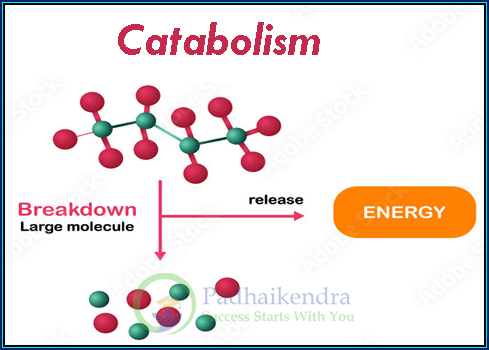
Picture external respiration as the ticket booth to a grand theater show, and cellular respiration as the star performance. The oxygen you inhale during external respiration is the opening act for the cellular respiration process.
Cellular Powerhouse: Cellular respiration is how your cells generate energy. It’s like the engine in a car, converting fuel into usable energy (in this case, adenosine triphosphate or ATP).
Oxygen’s Role: Oxygen is the critical ingredient for cellular respiration. Inside your cells, it combines with glucose (a type of sugar) through a series of chemical reactions. This process releases energy, which your cells use to perform various functions.
So, the oxygen you inhale during external respiration is the spark that ignites the cellular respiration fire, fueling all your body’s activities, from moving muscles to thinking thoughts.
- Oxygen Delivery to Tissues
Your bloodstream is the courier service responsible for delivering oxygen to every cell in your body. Here’s how it works:
Hemoglobin Transport: We’ve already met hemoglobin, the red blood cell’s MVP. Hemoglobin binds to oxygen in the lungs and becomes the oxygen delivery truck.
Capillary Exchange: As your blood flows through tiny capillaries, oxygen is released from hemoglobin and diffuses into the surrounding tissues. This ensures that even the farthest cells from your lungs get their oxygen fix.
Tissue Need: Your body is incredibly efficient at matching oxygen delivery to tissue needs. When you’re active, your muscles require more oxygen, and your body responds by increasing blood flow to those areas.
- Removal of Cellular Waste
Every superhero has a nemesis, and for oxygen, it’s carbon dioxide (CO2), a waste product of cellular respiration. Once your cells have extracted the energy they need, they produce CO2 as a byproduct.
Return Journey: CO2 is transported back to the lungs through your bloodstream. Remember the bicarbonate ions and carbaminohemoglobin we talked about earlier? They help carry CO2 safely back to your lungs.
Expiration: When you exhale, you’re not just releasing used air; you’re expelling the waste CO2 your cells produced. Your lungs act as the escape route for this gas, ensuring it doesn’t build up in your body and disrupt the delicate pH balance of your blood.
This interplay between external and internal respiration is an exquisite example of your body’s ability to maintain equilibrium. It’s a continuous, dynamic process that ensures your cells receive the oxygen they need for energy production and efficiently eliminates waste gases to keep your internal environment in balance.
As we wrap up our journey through the world of respiration, we’ve learned that every breath you take is a small but essential step in this intricate dance of life, fueling your every move and sustaining your existence.
- Adaptations in Different Environments
- High Altitude Respiratory Changes
- Diving and Underwater Respiration
- Adaptations in Different Environments: Breathing Beyond Borders
In our quest to understand the remarkable world of respiration, it’s time to embark on a journey to explore how our bodies adapt to different environments. From the thin air of high altitudes to the underwater wonderland of the ocean, let’s uncover the fascinating ways our respiratory system copes with these extreme conditions.
- High Altitude Respiratory Changes
Imagine climbing a mountain, and as you ascend, the air gets thinner, making each breath feel like a precious commodity. This is the reality of high-altitude environments, where the oxygen levels are lower, and our bodies need to adapt.
Increased Ventilation: When you ascend to higher altitudes, your body responds by increasing your breathing rate and depth. This helps you inhale more air and compensate for the lower oxygen concentration.
Erythropoiesis: Your body also stimulates the production of red blood cells, a process called erythropoiesis. These cells carry oxygen, and having more of them helps ensure a steady supply of oxygen to your tissues.
Symptoms: Some people may experience symptoms like shortness of breath, dizziness, and fatigue when they first arrive at high altitudes. This is known as altitude sickness and is a result of your body adjusting to the lower oxygen levels.
Over time, your body can acclimatize to higher altitudes, but it’s essential to take it slow and allow your respiratory system to adapt gradually.
- Diving and Underwater Respiration
Diving into the depths of the ocean is like entering an alien world, where the challenges of underwater respiration are vastly different from what we experience on land.
Pressure Changes: As you descend deeper into the water, the pressure increases significantly. This can affect your respiratory system in several ways.
Breathing Gas: Most divers use a breathing gas mixture that contains oxygen and other gases like nitrogen or helium. The composition of this gas changes as you dive to compensate for the increasing pressure, ensuring your body gets the oxygen it needs.
Equalizing Pressure: To prevent pressure-related injuries, like barotrauma, divers must equalize the pressure in their ears and sinuses regularly. This helps ensure that the delicate respiratory structures are not damaged by the increasing pressure.
Breath-Holding: Some divers, like free divers or pearl divers, rely on their ability to hold their breath for extended periods underwater. This requires specific training to maximize oxygen utilization and minimize the buildup of carbon dioxide.
Underwater respiration is a testament to the adaptability of the human body. Whether you’re soaring to great heights or exploring the ocean’s depths, your respiratory system can adjust to the demands of the environment, ensuring you can breathe comfortably and safely.
These adaptations in different environments remind us of the incredible versatility of the human body. From the thin air of mountaintops to the pressure-filled depths of the ocean, our respiratory system rises to the occasion, allowing us to explore and thrive in diverse settings.
Conclusion
In conclusion, the journey through the world of respiration has been a fascinating exploration of the intricate processes that keep us breathing, adapting, and thriving in various environments. From the everyday miracle of external respiration, where we inhale life-giving oxygen and expel waste carbon dioxide, to the inner workings of cellular respiration, which powers our bodies at the cellular level, the breath is an essential thread woven into the fabric of our existence.
We’ve delved into the mechanics of our respiratory system, from the anatomical wonders of the nasal cavity to the microscopic alveoli where the magic of gas exchange takes place. We’ve uncovered the regulatory mechanisms that keep our breathing finely tuned, ensuring our bodies receive the oxygen they need and effectively eliminate waste gases.
In our exploration, we’ve encountered challenges, from the respiratory disorders that can disrupt the breath’s harmony to the adaptations our bodies undergo when faced with different environments, such as high altitudes or the depths of the ocean. These adaptations remind us of the incredible resilience of the human body and its capacity to adjust to a wide range of conditions.
As we conclude this journey, we’re left with a profound appreciation for the breath that sustains us. It’s a reminder of the intricate design and adaptability of our bodies, enabling us to navigate the world and experience its wonders. So, whether you’re scaling mountains or exploring the depths of the ocean, remember that the breath is your constant companion, ensuring you can embrace every moment of life’s adventures.