- Introduction
What Is Dead Airspace?
Importance of Dead Airspace in Respiration
- Introduction
In the intricate world of breathing, there’s a term that often goes unnoticed but plays a crucial role – Dead Airspace. It sounds mysterious, but fear not, we’re here to shed light on this hidden player in respiration. So, what is Dead Airspace, and why does it matter in the grand scheme of breathing?
What Is Dead Airspace?
Imagine you take a deep breath. You inhale air filled with life-giving oxygen. But here’s the catch: not all the air you breathe in reaches the tiny air sacs where oxygen and carbon dioxide exchange happens. Some of it hangs around in your airways, not contributing to this vital exchange. This stagnant air is what we call “Dead Airspace.”
Dead Airspace consists of the parts of your respiratory system where there’s no gas exchange occurring. Think of it as a room filled with air that doesn’t participate in the breathing party. It’s like having guests at a party who just stand around without joining the dance floor – they’re present, but they’re not actively participating.
Importance of Dead Airspace in Respiration
Now that we know what Dead Airspace is, let’s explore why it matters. At first glance, it might seem like a bit of wasted space in our respiratory system, but it serves several critical functions:
Temperature and Humidity Regulation: Dead Airspace helps to condition the air you breathe. As you inhale, it warms and humidifies the incoming air, making it more comfortable for your delicate lung tissues. This ensures that when the air reaches the exchange zone in your lungs, it’s just right.
Protection: This area acts as a defense mechanism against harmful particles and pathogens in the air. The hairs and mucus in your airways trap these intruders, preventing them from reaching deeper into your lungs.
Buffer for Breathing Rate: Dead Airspace can also be seen as a buffer for rapid changes in your breathing rate. When you breathe faster, you may inhale a bit more of this “stale” air. This allows your body to maintain a balance between oxygen and carbon dioxide levels, preventing sudden shifts that could be harmful.
Anesthesia and Medical Procedures: In medical procedures, understanding Dead Airspace is crucial. Anesthetists use this knowledge to administer anesthesia effectively, ensuring that patients receive the right amount without complications.
Respiratory Disorders: In conditions like chronic obstructive pulmonary disease (COPD) or asthma, Dead Airspace can become more prominent, making it harder for individuals to get the oxygen they need. Understanding and managing it is essential for improving their breathing.
In summary, Dead Airspace may seem like an uninvited guest in the respiratory system, but it’s a necessary one. It helps regulate the air you breathe, protects your lungs, and keeps your breathing steady. So, the next time you take a breath, remember that not all air goes straight to the party – some of it is busy doing its essential jobs in Dead Airspace.
- Anatomy of the Respiratory System
Upper Respiratory Tract
Lower Respiratory Tract
Alveoli: The Site of Gas Exchange
- Anatomy of the Respiratory System
Now that we’ve acquainted ourselves with Dead Airspace, let’s embark on a journey through the remarkable world of the respiratory system. It’s like an intricate highway for air, where every part has its unique role to play.
Upper Respiratory Tract
Imagine this as the grand entrance to the respiratory system. It starts at your nose, the part most of us are well acquainted with. When you breathe in, air enters through your nostrils. But it’s not just a simple passageway.
Nasal Passages: These are the tunnels in your nose that air travels through. They are lined with tiny hair-like structures called cilia and are decked with mucous-producing cells. Together, they act as the system’s natural air purifiers, trapping dust, pollen, and other nasties.
Pharynx (Throat): Beyond your nasal passages, the air moves into your throat, or pharynx. It’s a crucial junction for both air and food, where the respiratory and digestive systems cross paths. It’s like the traffic controller of your body.
Larynx (Voice Box): Just below the pharynx, you’ll find the larynx. It houses your vocal cords, responsible for the magic of speech and singing. It also plays a protective role, closing up when you swallow to prevent food from going down the wrong pipe.
Lower Respiratory Tract
Now, let’s head deeper into the respiratory territory. As the air passes through the upper tract, it continues its journey:
Trachea (Windpipe): This is the highway for air, leading it to its next destination: the lungs. The trachea is like a sturdy tube made of rings of cartilage, keeping it open and preventing it from collapsing.
Bronchi: As we go further, the trachea splits into two bronchi, one leading to each lung. These are like the main roads that will take the air into different lung territories.
Bronchioles: Think of bronchioles as the smaller streets branching off from the bronchi. They keep dividing into even tinier passages, guiding the air deeper into the lungs.
Alveoli: The Site of Gas Exchange
Now, we’ve reached the final destination, the place where all the magic happens – the alveoli. These are like tiny, grape-like sacs that cover the innermost part of your lungs. If your lungs were a bustling city, the alveoli would be the factories where the exchange of oxygen and carbon dioxide takes place.
Here’s how it works: Oxygen from the air you breathe in passes through the walls of the alveoli into your bloodstream. At the same time, carbon dioxide, a waste product, travels from your blood into the alveoli to be exhaled out of your body. This exchange powers your body with the oxygen it needs and removes the waste gases.
So, next time you take a breath, remember the intricate journey your body undertakes to make sure you get the oxygen you need. From the grand entrance of your nose to the tiny factories of the alveoli, every part plays a vital role in keeping you alive and well.
III. Dead Airspace: Definition and Significance
Definition of Dead Airspace
Why Dead Airspace Matters
III. Dead Airspace: Definition and Significance
As we venture further into the world of respiration, it’s time to shine a spotlight on Dead Airspace – that enigmatic zone within our respiratory system. What exactly is Dead Airspace, and why should we care about it? Let’s uncover the secrets.
Definition of Dead Airspace
Dead Airspace, despite its somewhat cryptic name, is quite straightforward. Imagine you’re in a crowded room, but not everyone is part of the conversation. Some folks are just there, not contributing to the lively chatter. In your respiratory system, Dead Airspace is that room.
It’s the space where the inhaled air doesn’t actively participate in the crucial exchange of oxygen and carbon dioxide. Instead, it lingers in your airways, taking a breather, so to speak. This air is still, not in motion, and doesn’t join the respiratory party happening in your alveoli, the tiny sacs where oxygen and carbon dioxide trade places.
Why Dead Airspace Matters
Now, you might wonder why we’re bothering with this seemingly idle air. Well, Dead Airspace might not be the life of the breathing party, but it serves several vital roles:
- Temperature and Humidity Control: Think of Dead Airspace as your system’s air conditioner and humidifier. When you inhale, this air helps to warm up and moisten the incoming oxygen. By the time the air reaches the deeper regions of your lungs, it’s just the right temperature and humidity for your sensitive lung tissues.
- Shield Against Invaders: Dead Airspace isn’t just a quiet corner; it’s also a guardian. Dust, pollen, and potentially harmful particles in the air get trapped in this zone. It’s like a bouncer keeping the troublemakers away from the VIP area of your lungs.
- Keeping Breathing Steady: Dead Airspace also acts as a buffer for your breathing rate. When you breathe faster (say, after a run), you might inhale a bit more of this “stale” air. It’s a clever way your body maintains a balance between oxygen and carbon dioxide levels, preventing sudden shifts that could harm you.
- Anesthesia and Medical Procedures: In the world of medicine, understanding Dead Airspace is essential. Anesthesiologists use this knowledge to administer anesthesia effectively, ensuring patients get just the right amount without complications.
- Respiratory Disorders: In conditions like COPD or asthma, Dead Airspace becomes more noticeable. It can make it harder for individuals to get the oxygen they need. Understanding and managing it are crucial for improving their breathing and quality of life.
So, while Dead Airspace might seem like the wallflower at the respiratory ball, it’s an essential part of the respiratory system dance. It regulates the air you breathe, protects your lungs, and helps maintain the harmony of your breathing. The next time you take a breath, remember that not all air reaches the spotlight – some of it plays a vital behind-the-scenes role in Dead Airspace.
- Factors Affecting Dead Airspace
Age and Dead Airspace
Respiratory Conditions and Dead Airspace
Environmental Factors
Medical Interventions
- Factors Affecting Dead Airspace
In our journey through the respiratory realm, we’ve met Dead Airspace, that quiet corner where not all inhaled air joins the respiratory hustle. But now, let’s dive deeper and understand what affects the size and role of this airspace. Age, respiratory conditions, the environment, and medical interventions all play a part.
Age and Dead Airspace
Age is like the master conductor of the respiratory orchestra. As we grow from tiny tots to wise elders, our respiratory system undergoes changes. This includes alterations in Dead Airspace:
Infants and Children: In the early chapters of life, little lungs are still growing and developing. This means a proportionally larger Dead Airspace, which gradually reduces as they mature.
Adults: As we hit adulthood, our respiratory system reaches its peak efficiency. The Dead Airspace is relatively stable during this period.
Elderly: In the later years, the respiratory system experiences wear and tear. Dead Airspace may increase slightly due to factors like reduced lung elasticity. It’s like the wrinkles that come with age, but in the world of respiration.
Respiratory Conditions and Dead Airspace
Here’s where the plot thickens. Certain respiratory conditions can alter the Dead Airspace equation:
Chronic Obstructive Pulmonary Disease (COPD): In this condition, the airways become narrower and obstructed. This can increase Dead Airspace, making it harder for individuals to get the oxygen they need.
Asthma: Asthma, with its spasms of the airways, can also influence Dead Airspace. During an asthma attack, more air can be trapped in the respiratory passages, contributing to Dead Airspace.
Environmental Factors
Nature’s elements also have a say in the size and significance of Dead Airspace:
Altitude: The higher you go, the thinner the air becomes. At high altitudes, there’s less oxygen available, and Dead Airspace may play a more prominent role in ensuring the air you breathe is adequately prepared for your body’s needs.
Temperature: Extreme temperatures can impact how Dead Airspace functions. In cold conditions, the air needs extra warming, which can increase Dead Airspace’s workload.
Humidity: Dry air can be harsh on your respiratory system. Dead Airspace helps by humidifying the inhaled air, making it more comfortable for your lungs.
Medical Interventions
Sometimes, medical wizards need to step in to ensure the respiratory show goes on smoothly. Here’s how they do it:
Ventilation Strategies: In medical settings, ventilation machines can be used to manage Dead Airspace. These machines ensure a consistent supply of oxygen, even if a patient’s respiratory system isn’t operating at full capacity.
Breathing Apparatus: Devices like respirators or ventilators can also be employed to assist with breathing. These devices take over when the respiratory system needs a helping hand, often bypassing Dead Airspace to provide oxygen directly to the lungs.
So, as we explore the factors affecting Dead Airspace, remember that this seemingly quiet corner of the respiratory system is influenced by a myriad of factors. Age, conditions, the environment, and medical interventions all play their part in ensuring that the air you breathe is just right for your body’s needs. It’s like a symphony, where each instrument has a role to play in the harmony of respiration.
- Measuring Dead Airspace
Methods for Measuring Dead Airspace
Clinical Applications
- Measuring Dead Airspace
Our journey through the respiratory labyrinth continues, and now we’re turning our attention to a crucial aspect: measuring Dead Airspace. Just as you’d use a map to navigate unfamiliar terrain, these measurements help us understand and manage this enigmatic space. So, let’s explore the methods used and why they matter in clinical settings.
Methods for Measuring Dead Airspace
Body Plethysmography: Imagine you’re inside a sealed box, and you try to take a deep breath. Body plethysmography is somewhat like that. It measures the change in pressure inside a closed chamber when you breathe in and out. By monitoring this pressure change, it calculates the volume of your lungs, including Dead Airspace.
Nitrogen Washout Test: This test involves breathing in 100% oxygen for a brief period. Oxygen doesn’t participate in the gas exchange in Dead Airspace because it’s not absorbed by your body. So, the concentration of nitrogen in your exhaled breath helps calculate the Dead Airspace volume.
Bohr Dead Space Equation: Named after the Danish physiologist Christian Bohr, this equation estimates Dead Airspace by analyzing the ratio of carbon dioxide in exhaled air to carbon dioxide in arterial blood. It provides valuable insights into lung function.
Capnography: This method measures the concentration of carbon dioxide (CO2) in the exhaled air. By analyzing the CO2 levels, clinicians can gain insights into Dead Airspace, especially during anesthesia and critical care situations.
Clinical Applications
Now that we’ve learned how to measure Dead Airspace, let’s dive into why these measurements matter in the world of medicine:
Respiratory Disorders: Understanding Dead Airspace is crucial in diagnosing and managing respiratory conditions like chronic obstructive pulmonary disease (COPD) and asthma. Measuring Dead Airspace helps clinicians assess the severity of these conditions and tailor treatment plans accordingly.
Ventilation Management: During mechanical ventilation, it’s essential to monitor Dead Airspace. If too much air bypasses the alveoli (the gas exchange units of the lungs) and remains in Dead Airspace, it can lead to inefficient ventilation and potential complications. Measurements help fine-tune ventilator settings.
Anesthesia: In the realm of anesthesia, knowing Dead Airspace is vital. Anesthesiologists use these measurements to determine the appropriate dosage of anesthesia drugs, ensuring patient safety during surgical procedures.
Monitoring Respiratory Efficiency: Continuous monitoring of Dead Airspace can provide valuable information about a patient’s respiratory efficiency. It allows healthcare providers to make real-time adjustments to optimize oxygen delivery and carbon dioxide removal.
Research and Advancements: Measurements of Dead Airspace contribute to ongoing research in respiratory medicine. They help scientists better understand the intricacies of lung function, leading to advancements in diagnosis and treatment.
In summary, measuring Dead Airspace is like shining a flashlight in a dark corner of the respiratory system. It helps healthcare professionals assess lung function, diagnose disorders, manage ventilation, and enhance patient care. As technology advances and our understanding of respiratory physiology deepens, these measurements continue to play a vital role in ensuring healthy breathing and well-being.
- Clinical Relevance
Dead Airspace and Ventilation
Implications in Respiratory Distress
Anesthesia and Intubation Considerations
- Clinical Relevance
As our journey into the world of Dead Airspace continues, it’s time to explore its clinical relevance. This seemingly quiet corner of the respiratory system has significant implications for various aspects of healthcare, from ventilation strategies to managing respiratory distress and even considerations during anesthesia and intubation.
Dead Airspace and Ventilation
Imagine trying to inflate a balloon, but instead of air filling the balloon, it just goes into the surrounding space. That’s a bit like what can happen when Dead Airspace is not properly managed during ventilation.
Ventilation, in medical terms, is the process of moving air in and out of the lungs, ensuring that oxygen gets to where it’s needed and carbon dioxide is removed. Dead Airspace can pose a challenge here. If a significant portion of the air isn’t reaching the gas-exchanging alveoli in the lungs and instead remains in the non-participatory zones, it can lead to inefficient ventilation.
Understanding Dead Airspace is crucial for healthcare professionals, especially when patients require mechanical ventilation. By factoring in Dead Airspace measurements, they can fine-tune ventilator settings to ensure that enough oxygen reaches the alveoli and that carbon dioxide is efficiently removed.
Implications in Respiratory Distress
When someone is in respiratory distress, every breath counts. Dead Airspace can become a more prominent player in such situations.
In conditions like chronic obstructive pulmonary disease (COPD) or asthma, where the airways are obstructed and airflow is limited, Dead Airspace can contribute to the feeling of breathlessness. It’s like trying to fill a bottle with a narrow neck – not all the air gets in. In these cases, healthcare providers need to carefully manage Dead Airspace to optimize oxygen delivery to the patient.
Anesthesia and Intubation Considerations
Think of anesthesia as temporarily hitting the pause button on your body’s awareness. During surgery or medical procedures, patients often receive anesthesia to ensure they don’t feel pain or move. However, when administering anesthesia, it’s crucial to consider Dead Airspace.
Anesthesiologists need to calculate the appropriate dosage of anesthesia drugs based on factors like a patient’s age, weight, and lung function, including Dead Airspace. If Dead Airspace is not factored in, there’s a risk of under or overmedication, which can lead to complications during the procedure.
Additionally, when it comes to intubation (inserting a tube into the airway to assist with breathing), understanding Dead Airspace helps ensure that the tube placement is optimal. It ensures that the air supplied through the tube effectively reaches the lungs and doesn’t get trapped in the non-exchanging regions.
In conclusion, Dead Airspace may seem like a silent character in the respiratory play, but its clinical relevance is anything but insignificant. It impacts ventilation strategies, plays a role in respiratory distress, and demands careful consideration in anesthesia and intubation. Healthcare professionals rely on this understanding to provide efficient and safe care, ensuring that every breath counts in the quest for well-being.
VII. Dead Airspace in Respiratory Disorders
COPD and Dead Airspace
Asthma and Dead Airspace
Pneumonia and Dead Airspace
Ventilation-Perfusion Mismatch
VII. Dead Airspace in Respiratory Disorders
Our exploration of Dead Airspace takes us deeper into the world of respiratory disorders. In this chapter, we’ll uncover how conditions like COPD, asthma, pneumonia, and the intriguing ventilation-perfusion mismatch interact with Dead Airspace.
COPD and Dead Airspace
Chronic Obstructive Pulmonary Disease (COPD) is like a dragon that challenges the respiratory system. In COPD, the airways become narrow and obstructed, making it harder to breathe. Dead Airspace steps into the spotlight here.
Increased Dead Airspace: COPD can lead to an increase in Dead Airspace. The narrowed airways mean that a larger portion of the inhaled air doesn’t make it to the gas-exchanging alveoli. This can result in insufficient oxygen reaching the bloodstream, leading to breathlessness and fatigue.
Ventilation-Perfusion Mismatch: COPD often causes a mismatch between ventilation (airflow) and perfusion (blood flow) in the lungs. This means that while some areas of the lung receive air, they don’t receive enough blood, and vice versa. Dead Airspace can exacerbate this mismatch, further reducing the effectiveness of breathing.
Asthma and Dead Airspace
Asthma, on the other hand, is like a rollercoaster ride for the airways, with sudden ups and downs. It involves periodic spasms of the airways, and Dead Airspace plays a role here too.
Increased Dead Airspace During Attacks: During an asthma attack, the airways constrict and become inflamed, leading to more air being trapped in Dead Airspace. This trapped air contributes to the sensation of breathlessness and can make it challenging for individuals to get the oxygen they need.
Managing Dead Airspace: Understanding Dead Airspace is crucial in managing asthma. Medications like bronchodilators aim to reduce airway constriction, which can help decrease Dead Airspace and improve airflow to the alveoli.
Pneumonia and Dead Airspace
Pneumonia is like an unwanted guest in the lungs – it brings inflammation and infection. Dead Airspace intersects with pneumonia in a unique way:
Alveoli Filling with Fluid: In pneumonia, the alveoli (the tiny sacs responsible for gas exchange) often fill with fluid and inflammatory debris. This reduces the effective space for gas exchange, pushing Dead Airspace into the spotlight. It becomes more challenging for oxygen to reach the bloodstream.
Efficiency Is Key: Healthcare providers focus on making breathing as efficient as possible for pneumonia patients. Dead Airspace measurements can guide them in tailoring treatment strategies to maximize oxygen delivery.
Ventilation-Perfusion Mismatch
The ventilation-perfusion (V/Q) ratio is like the harmony between airflow (ventilation) and blood flow (perfusion) in the lungs. When this balance is disrupted, it can lead to significant respiratory challenges.
Impact on Dead Airspace: A V/Q mismatch can result in areas of the lung receiving ventilation but not enough blood flow, and vice versa. In cases where there’s adequate ventilation but reduced perfusion, Dead Airspace becomes more prominent.
Diagnostic Insights: Dead Airspace measurements can provide valuable diagnostic insights in conditions characterized by V/Q mismatch, helping healthcare providers identify the source of the problem and develop targeted treatment plans.
In conclusion, Dead Airspace is like a silent character that takes on different roles in various respiratory disorders. In COPD and asthma, it can exacerbate breathlessness, while in pneumonia, it competes with inflamed alveoli. Understanding Dead Airspace is essential for tailoring treatment strategies and providing optimal care to individuals dealing with these respiratory challenges. Moreover, it sheds light on the intricate balance of ventilation and perfusion in the lungs, offering valuable insights for diagnosis and treatment.
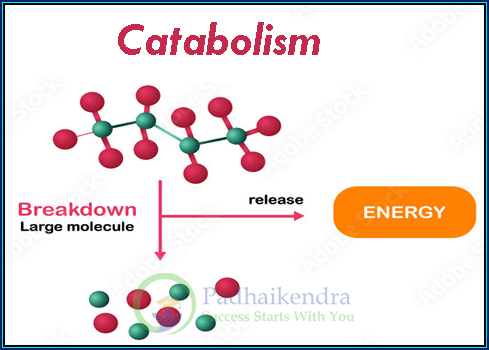
VIII. Managing Dead Airspace
Therapeutic Approaches
Preoperative and Postoperative Considerations
VIII. Managing Dead Airspace
In our journey through the mysteries of the respiratory system, we’ve reached a critical juncture: managing Dead Airspace. It’s time to explore the strategies and considerations when dealing with this enigmatic space, both before and after medical procedures.
Therapeutic Approaches
Managing Dead Airspace involves a combination of strategies aimed at optimizing breathing efficiency and ensuring that the right amount of oxygen reaches the gas-exchanging alveoli in the lungs.
Positive End-Expiratory Pressure (PEEP): PEEP is like a gentle helping hand for your lungs. It’s a technique used in mechanical ventilation where a small amount of positive pressure is applied to the airways at the end of each breath. This keeps the airways open and prevents them from collapsing, especially in individuals with conditions like COPD. By doing so, it reduces Dead Airspace and improves the exchange of oxygen and carbon dioxide.
Mechanical Ventilation: In cases where a patient’s respiratory system is compromised, such as during surgery or in critical care settings, mechanical ventilation can come to the rescue. Ventilators provide a controlled supply of air, ensuring that Dead Airspace is minimized, and adequate oxygen is delivered to the alveoli.
Preoperative Considerations: Before undergoing surgery, individuals with pre-existing respiratory conditions need special attention. Healthcare providers assess their lung function, including Dead Airspace, to determine the most suitable anesthesia and ventilation strategies. This helps ensure a safe and successful procedure.
Postoperative Monitoring: After surgery, individuals are closely monitored, and Dead Airspace measurements can continue to be useful. Monitoring helps healthcare providers assess how well a patient is recovering and whether adjustments to ventilation or oxygen support are necessary.
Preoperative and Postoperative Considerations
Surgery is like embarking on a journey, and managing Dead Airspace is an essential part of the preparations and recovery process.
Preoperative Assessment: Before surgery, individuals with respiratory conditions undergo a thorough evaluation. This includes assessing lung function, measuring Dead Airspace, and considering any potential challenges related to anesthesia and ventilation during the procedure.
Tailored Anesthesia: Anesthesiologists are like air traffic controllers during surgery. They carefully calculate the dosage of anesthesia drugs, factoring in Dead Airspace measurements and individual patient factors. This ensures that the patient remains comfortably sedated and safe throughout the procedure.
Ventilation Strategies: During surgery, mechanical ventilation may be employed. It’s a bit like having a backup breathing system. Ventilators deliver oxygen and help remove carbon dioxide, all while managing Dead Airspace to ensure optimal lung function.
Postoperative Care: After the procedure, individuals are closely monitored in the recovery room. Monitoring includes assessing breathing patterns and oxygen levels. Any changes or challenges related to Dead Airspace are addressed promptly to ensure a smooth recovery.
In conclusion, managing Dead Airspace is like orchestrating a symphony in the respiratory system. Therapeutic approaches like PEEP and mechanical ventilation, along with careful preoperative and postoperative considerations, are vital for optimizing lung function and ensuring patient well-being during surgical procedures. By understanding the nuances of Dead Airspace, healthcare providers can provide the best care, ensuring that each breath contributes to a successful recovery.
- Research and Advances
Studies on Dead Airspace Reduction
Emerging Technologies
Future Directions in Respiratory Medicine
- Research and Advances
As we journey through the realm of Dead Airspace, we must also cast our gaze towards the future. In this chapter, we’ll delve into the ongoing studies, emerging technologies, and the exciting possibilities that lie ahead in the field of respiratory medicine.
Studies on Dead Airspace Reduction
Researchers are like explorers, always seeking ways to improve our understanding and management of Dead Airspace. They’re on a mission to reduce Dead Airspace and enhance respiratory care.
Pharmacological Interventions: Scientists are exploring medications that can help reduce airway constriction and inflammation. By doing so, they aim to minimize Dead Airspace in conditions like COPD and asthma.
Ventilator Innovations: In the world of mechanical ventilation, researchers are developing smarter and more adaptive ventilators. These devices aim to optimize air distribution within the lungs, minimizing Dead Airspace and improving oxygen delivery.
Personalized Medicine: The future of healthcare is personalized. Researchers are working on tailoring treatment plans based on an individual’s unique respiratory profile, including Dead Airspace measurements. This could lead to more effective and targeted therapies.
Emerging Technologies
Technology is like a beacon of hope in the world of medicine, and it’s making waves in Dead Airspace management.
Advanced Imaging: High-resolution imaging techniques, like magnetic resonance imaging (MRI) and computed tomography (CT), are becoming more sophisticated. They allow for detailed visualization of the respiratory system, helping clinicians assess Dead Airspace more accurately.
Wearable Devices: Wearable technology is entering the respiratory arena. Devices that monitor breathing patterns and Dead Airspace in real-time are on the horizon. These gadgets could provide valuable insights for both individuals with respiratory conditions and healthcare providers.
Artificial Intelligence (AI): AI algorithms are being trained to analyze medical data, including Dead Airspace measurements, more efficiently. This could streamline diagnosis and treatment recommendations, leading to faster and more precise care.
Future Directions in Respiratory Medicine
The future is bright for respiratory medicine, and Dead Airspace is no exception. Here’s what the crystal ball shows:
Precision Medicine: We’re moving towards a future where respiratory care is tailored to each person’s unique needs. Dead Airspace measurements will play a pivotal role in these personalized treatment plans.
Telemedicine: Remote healthcare is on the rise. With the help of telemedicine, individuals with respiratory conditions can receive ongoing care and guidance, including Dead Airspace monitoring, from the comfort of their homes.
Preventive Strategies: The best way to deal with respiratory disorders is to prevent them. Future research may uncover ways to identify individuals at risk for conditions related to Dead Airspace early on, allowing for preventive interventions.
Global Impact: Respiratory health is a global concern. Research and advances in Dead Airspace management will have far-reaching implications, especially in regions with a high burden of respiratory diseases.
In conclusion, the future of Dead Airspace is teeming with promise. Ongoing studies are unraveling its mysteries, and emerging technologies are poised to revolutionize respiratory care. With precision medicine, telemedicine, and a focus on prevention, the horizon of respiratory medicine looks brighter than ever. Dead Airspace, once a silent character in the respiratory play, is stepping into the spotlight, ready to contribute to healthier breathing and improved well-being for all.
Conclusion
In conclusion, our journey through the intricate world of Dead Airspace has revealed its significance and relevance in the realm of respiratory medicine. From its definition and role in respiration to its impact on various respiratory disorders, Dead Airspace has proven to be a character with depth and importance.
We’ve explored how Dead Airspace can affect ventilation, its implications in respiratory distress, and its critical role in anesthesia and intubation procedures. Managing Dead Airspace involves a symphony of strategies, from positive end-expiratory pressure to tailored anesthesia and vigilant postoperative care.
As we peer into the future, research continues to unlock the secrets of Dead Airspace, offering innovative solutions to reduce its impact and improve respiratory care. Emerging technologies like advanced imaging, wearable devices, and artificial intelligence are poised to revolutionize the way we understand and manage this crucial aspect of breathing.
In the ever-evolving landscape of respiratory medicine, Dead Airspace is stepping into the limelight, ready to play a leading role in personalized, preventive, and globally impactful approaches to respiratory health. With each breath, it reminds us that even the quietest corners of our body can hold the key to a healthier and brighter future.