- Introduction to the Seminal Vesicle
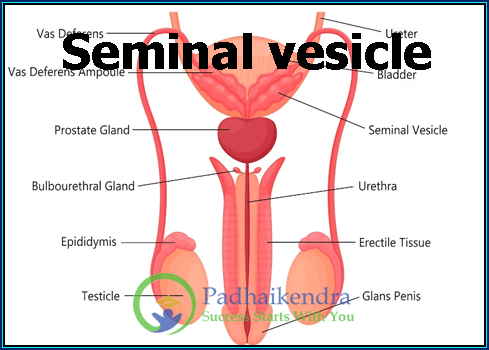
- Definition and Anatomy
- Location and Size
- Histology and Structure
- Introduction to the Seminal Vesicle
Welcome to the fascinating world of the seminal vesicle! In this article, we’ll dive into the ins and outs of this vital part of the male reproductive system, breaking down everything you need to know in simple and unique language.
- Definition and Anatomy
Let’s start with the basics. The seminal vesicle is a small but mighty organ found in the male reproductive system. Picture it as a reservoir that holds an essential ingredient for creating life: the seminal fluid. This fluid is not to be confused with sperm; instead, it’s the stuff that supports and nourishes sperm during their journey to meet the egg.
Now, let’s talk about where this little powerhouse is located. You can find the seminal vesicle in the pelvis, tucked right behind the bladder and above the prostate gland. It’s like a neighbor that lives next door to the bladder. Size-wise, these vesicles are typically around 2 to 5 inches long, and they come in a pair, one on each side.
- Location and Size
Imagine your bladder as a water balloon. Right above it, you’ll find the seminal vesicles hanging out, like small, squishy pouches. They are strategically placed there because they play a crucial role in the journey of sperm. When it’s time for ejaculation, these vesicles release their special fluid into the mix, making up a significant part of what we commonly call semen.
- Histology and Structure
Now, let’s get a bit closer to what’s happening inside these vesicles. If you were to zoom in with a microscope, you’d see that they are made up of different layers of cells and tissues. It’s like a tiny factory, busy at work. The walls of the seminal vesicles contain smooth muscle cells, which help them contract and squeeze out their contents during ejaculation.
Inside these vesicles, there are glands that produce the magical fluid. This fluid isn’t just water; it’s packed with nutrients and substances that give sperm the energy and protection they need for their journey. You can think of it as a packed lunch for sperm, providing them with the sustenance they need to swim and survive.
So, to sum it up, the seminal vesicle is a small, pouch-like structure located near the bladder, about the size of your fingers. It’s responsible for producing a special fluid that supports sperm on their quest to fertilize an egg. Inside, it’s like a little factory with different parts working together to create this vital fluid.
Now that we’ve laid the foundation, stay tuned as we explore the functions, development, and importance of the seminal vesicle in the next sections of this article.
- Functions of the Seminal Vesicle
- Seminal Fluid Production
- Nutrient Contribution to Semen
- Role in Fertilization
- Interaction with Prostate Gland
- Functions of the Seminal Vesicle
Welcome back to our exploration of the seminal vesicle! In this section, we’re going to uncover the incredible functions of this small but essential player in the male reproductive system. Get ready for a unique and straightforward journey.
- Seminal Fluid Production
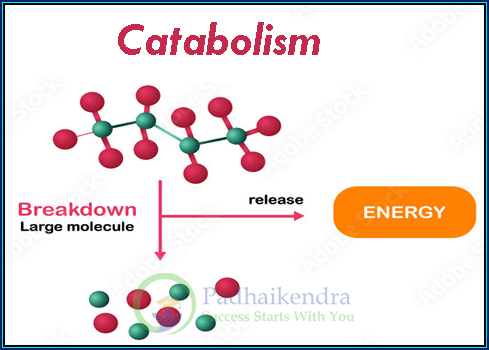
Alright, so let’s talk about what the seminal vesicle brings to the party. Its primary job is to produce a special, nutrient-rich fluid called seminal fluid. Think of it as the secret sauce that goes into making semen, which is the stuff that carries sperm on their adventure to meet an egg.
The seminal fluid isn’t just some plain old liquid; it’s loaded with goodies. We’re talking about fructose (a type of sugar), amino acids (the building blocks of proteins), and even enzymes. These ingredients might sound like something you’d find in a recipe, but they serve a vital purpose. The fructose provides energy for the sperm, the amino acids help keep them strong, and the enzymes help break down barriers within the female reproductive tract.
- Nutrient Contribution to Semen
You can think of the seminal vesicle as a chef that adds flavor and nutrients to the dish. When the seminal fluid mixes with sperm from the testes and a few other secret ingredients from the prostate gland, it becomes semen. This nutrient-rich cocktail is what nourishes and protects the sperm, ensuring they have the best chance at reaching and fertilizing an egg.
- Role in Fertilization
Now, let’s get into the nitty-gritty of why this seminal fluid is so crucial. When a man ejaculates, this mixture of semen and sperm travels through the male’s reproductive system and into the female’s reproductive tract during intercourse. The seminal fluid’s job is to provide the sperm with the nutrients and energy they need to make their long and treacherous journey towards the egg.
Think of it as a grand race. The sperm are the racers, and the seminal fluid is their energy drink. Without this special fluid, the sperm would tire out and never reach the finish line, which is the egg. So, in short, the seminal vesicle plays a starring role in helping sperm on their quest to fertilize an egg, which is the key to creating new life.
- Interaction with Prostate Gland
But wait, there’s a partner in crime! The seminal vesicle doesn’t work alone. It has a buddy called the prostate gland. These two organs work hand in hand to produce and release the components of semen. The prostate gland adds its own ingredients to the mix, such as enzymes and a milky fluid. Together, the seminal vesicle and the prostate gland create a balanced concoction that helps sperm survive and swim effectively.
So, there you have it. The seminal vesicle is like the chef in the kitchen, whipping up a delicious and nutritious meal for the sperm, while the prostate gland is the sous-chef adding its special touches. Together, they ensure that sperm are well-fed, protected, and ready for their epic journey to fertilize an egg.
In the next sections, we’ll explore the development of the seminal vesicle, common disorders, and how doctors diagnose and treat issues related to this fascinating organ. Stay tuned!
III. Development and Embryology
- Formation during Fetal Development
- Changes during Puberty
III. Development and Embryology
Welcome to the third chapter of our journey into the world of the seminal vesicle. In this section, we’ll unravel the fascinating story of how this tiny but mighty organ comes into existence during fetal development and undergoes changes during puberty. Get ready for a unique and simple exploration.
- Formation during Fetal Development
The story of the seminal vesicle begins even before you were born. When you were just a tiny, developing fetus, your body was busy creating all the parts needed for your future life. Among these parts is the seminal vesicle. It’s a bit like building a puzzle; every piece has its role to play.
The seminal vesicle starts as these small, bud-like structures that eventually grow into the pouch-like organs we now know. These buds form from the same tissue that gives rise to the male reproductive system, and as the fetus develops, they begin to take shape and grow.
It’s amazing to think that even before you were born, the groundwork for your future reproductive abilities was being laid. The seminal vesicles were a part of this intricate process, quietly waiting for their moment to shine.
- Changes during Puberty
Fast forward a bit, and we arrive at puberty, that remarkable time when a young boy transforms into a young man. The seminal vesicle doesn’t just remain static; it undergoes changes as well. It’s like the final touches being added to a masterpiece.
During puberty, the male body experiences a surge in hormones, particularly testosterone. This hormone acts as a catalyst, triggering several changes. One of the pivotal changes involves the seminal vesicle. It starts to produce and store the seminal fluid we discussed earlier, getting it ready for its future role in reproduction.
As a young man progresses through puberty, his seminal vesicles grow in size and become more active. They begin contributing to the semen, which means they start producing that essential nutrient-rich fluid. This marks the beginning of a young man’s ability to father children.
In a nutshell, the seminal vesicle is like a quiet hero that gets its start during fetal development, patiently waiting for puberty to kick in. When the time comes, it transforms, grows, and becomes an essential part of the male reproductive system.
In the upcoming sections, we’ll delve into common disorders related to the seminal vesicle and how doctors diagnose and treat these issues. So, stay with us on this journey through the wonders of the male reproductive system!
- Common Disorders and Conditions
- Seminal Vesiculitis
- Seminal Vesicle Cysts
- Seminal Vesicle Calculi (Stones)
- Seminal Vesicle Agenesis
- Cancer of the Seminal Vesicle (Rare)
- Common Disorders and Conditions
Welcome to the next chapter in our exploration of the seminal vesicle. Just like any other part of the body, this tiny organ can sometimes face issues. In this section, we’ll discuss some common disorders and conditions that can affect the seminal vesicle. Let’s dive in, using simple and unique language.
- Seminal Vesiculitis
First up, we have a condition called seminal vesiculitis. Think of it as a sore throat for the seminal vesicle. Seminal vesiculitis occurs when these little pouches become inflamed or infected. It’s like having a mini battlefield inside your reproductive system.
The symptoms of seminal vesiculitis can include pain in the lower abdomen or pelvis, discomfort during ejaculation, and even pain in the lower back. Luckily, it’s usually treatable with antibiotics to clear up the infection and relieve the discomfort.
- Seminal Vesicle Cysts
Imagine a little bubble or pocket forming inside one of your seminal vesicles. That’s essentially what happens with seminal vesicle cysts. These cysts are fluid-filled sacs that can develop in the seminal vesicles, sometimes without any symptoms at all.
However, if they do cause problems, they can lead to pain in the pelvis, difficulty urinating, or discomfort during ejaculation. Treatment options depend on the size and severity of the cyst but may include medication or, in rare cases, surgery to remove the cyst.
- Seminal Vesicle Calculi (Stones)
Stones in the seminal vesicles? Yes, it’s possible. Seminal vesicle calculi, also known as stones, are tiny, solid masses that can form inside these pouches. They’re a bit like kidney stones but in a different place.
These little stones can cause discomfort and pain, especially during ejaculation. In some cases, they may need to be removed surgically, but often, they can be managed with medication and lifestyle changes.
- Seminal Vesicle Agenesis
Now, here’s a rare condition: seminal vesicle agenesis. This means that someone is born without one or both seminal vesicles. It’s like missing a puzzle piece.
Though it’s quite uncommon, this condition can affect a person’s fertility because the seminal vesicles play a significant role in producing the fluid that supports sperm. Treatment for this condition depends on the individual’s specific situation and fertility goals.
- Cancer of the Seminal Vesicle (Rare)
While exceedingly rare, cancer can affect the seminal vesicle. This is like finding a unicorn in the forest – it doesn’t happen often. When it does, it may cause symptoms such as blood in semen, pelvic pain, or changes in urination habits.
Treatment for cancer of the seminal vesicle may involve surgery, radiation therapy, or chemotherapy, depending on the extent of the disease.
In summary, the seminal vesicle, despite its small size, can face a range of conditions, from infections to cysts, stones, and even the rare occurrence of cancer. Thankfully, most of these conditions can be diagnosed and treated with the help of medical professionals. If you ever experience symptoms or have concerns about your reproductive health, it’s essential to seek medical advice and guidance.
- Diagnostic Procedures and Imaging
- Clinical Symptoms
- Physical Examination
- Laboratory Tests
- Imaging Techniques (Ultrasound, MRI, CT)
- Diagnostic Procedures and Imaging
Welcome to the next chapter of our journey into the world of the seminal vesicle. In this section, we’ll explore the various ways doctors diagnose and get a closer look at this tiny but essential organ. So, let’s dive into the world of diagnostic procedures and imaging, using simple and unique language.
- Clinical Symptoms
Sometimes, your body tries to tell you when something’s not quite right, and this can be the case with the seminal vesicle. If you’re experiencing issues like pelvic pain, discomfort during ejaculation, or changes in urination habits, these could be signs that something’s amiss. These are your body’s way of waving a red flag.
When you notice these symptoms, it’s crucial to reach out to a healthcare professional. They’ll listen to your concerns and help guide you through the diagnostic process to figure out what’s going on with your seminal vesicle.
- Physical Examination
Imagine going for a checkup, but this time, the doctor pays special attention to your lower abdomen and pelvis. That’s what a physical examination for the seminal vesicle might look like.
During this exam, your healthcare provider will use their trained hands to feel for any abnormalities or tenderness in the area. It’s a bit like a detective trying to gather clues to solve a mystery. The information they gather from this examination can be valuable in diagnosing conditions like seminal vesiculitis or cysts.
- Laboratory Tests
When your body is trying to tell you something’s up, sometimes it leaves hints in your bodily fluids. This is where laboratory tests come into play. Doctors may ask for a sample of your urine or semen to check for signs of infection or other issues related to the seminal vesicle.
These tests can help provide a clearer picture of what’s happening inside your body. It’s like putting together pieces of a puzzle to see the bigger picture.
- Imaging Techniques (Ultrasound, MRI, CT)
Now, it’s time to bring in the big guns – imaging techniques. These are like the superhero tools that can peer inside your body and reveal what’s happening with your seminal vesicle.
Ultrasound: Think of this as using sound waves to create a picture. It’s painless and non-invasive. An ultrasound can show the size, shape, and any abnormalities in the seminal vesicle.
MRI (Magnetic Resonance Imaging): This is like having your body’s internal structures photographed with powerful magnets and radio waves. An MRI can provide detailed images of the seminal vesicle and nearby structures, helping doctors see if anything is amiss.
CT (Computed Tomography): Imagine slicing a loaf of bread into thin pieces to examine each one individually. CT scans are a bit like that, creating cross-sectional images of the body. They can be useful in diagnosing conditions like seminal vesicle stones or tumors.
In conclusion, diagnosing issues related to the seminal vesicle involves a combination of clinical symptoms, physical examinations, laboratory tests, and advanced imaging techniques. These tools and procedures help doctors get to the bottom of any problems and guide the way to appropriate treatments and solutions. So, if you ever have concerns about your reproductive health, don’t hesitate to seek professional advice and care.
- Treatment and Management
- Medical Interventions
- Antibiotics for Infections
- Pain Management
- Surgical Procedures
- Drainage of Cysts
- Surgical Removal (Rarely)
- Lifestyle Changes and Prevention
- Treatment and Management
Welcome to the next chapter in our exploration of the seminal vesicle. In this section, we’ll delve into the various ways to treat and manage conditions related to this important but often overlooked organ. Get ready for a journey through medical interventions, surgical procedures, and even some lifestyle tips, all explained in simple and unique language.
- Medical Interventions
Antibiotics for Infections
When it comes to treating conditions like seminal vesiculitis, where the seminal vesicle becomes inflamed or infected, antibiotics are like the superheroes that come to the rescue. These medications are specially designed to fight off the bad guys (bacteria) causing the infection.
Doctors will prescribe antibiotics based on the type of infection and its severity. Taking the full course of antibiotics as directed is crucial to ensure that all the bacteria are defeated and the infection is properly treated.
Pain Management
Imagine having a sore back or pelvis because of an issue with your seminal vesicle. Pain management techniques can help ease the discomfort and make you feel better. This could involve over-the-counter pain relievers like ibuprofen or more potent medications prescribed by a healthcare professional.
The goal of pain management is to improve your quality of life while your body heals. It’s like having a soothing balm for your discomfort.
- Surgical Procedures
Drainage of Cysts
If you have a pesky cyst in your seminal vesicle causing problems, a doctor might recommend draining it. It’s like popping a balloon, but a lot more controlled.
During this procedure, a healthcare provider will use a needle or catheter to remove the fluid from the cyst, relieving any pain or pressure it might be causing. It’s a relatively simple procedure that can provide significant relief.
Surgical Removal (Rarely)
Sometimes, conditions in the seminal vesicle might be more stubborn, like large or complicated cysts, or even very rare cases of cancer. In these instances, surgical removal of the seminal vesicle may be considered. It’s like removing a malfunctioning part from a machine to ensure everything runs smoothly.
This procedure is usually a last resort and is only performed when other treatments have not been effective. It’s a more complex surgery and typically requires a longer recovery period.
- Lifestyle Changes and Prevention
Prevention is always better than cure, right? When it comes to your seminal vesicle, there are some lifestyle changes and habits that can help keep it healthy:
Safe Sex: Practicing safe sex can reduce the risk of sexually transmitted infections that could affect your seminal vesicle.
Stay Hydrated: Drinking plenty of water can help prevent the formation of stones in the seminal vesicle.
Regular Check-Ups: Just like you’d take your car for regular maintenance, seeing a doctor for routine check-ups can catch potential issues early.
Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can contribute to overall reproductive health.
In conclusion, the treatment and management of seminal vesicle-related conditions involve a range of options, from antibiotics and pain management to surgical procedures in rare cases. And don’t forget, a healthy lifestyle and preventive measures can go a long way in keeping your seminal vesicle and your overall reproductive health in top shape. So, take care of yourself, and don’t hesitate to seek medical advice if needed.
VII. Importance of Seminal Vesicles in Reproductive Health
- Fertility Implications
- Impact on Sexual Function
- Research and Future Developments
VII. Importance of Seminal Vesicles in Reproductive Health
Welcome to the heart of our exploration into the seminal vesicle. In this section, we’ll uncover the crucial role these small but mighty organs play in reproductive health. Buckle up for a journey through their impact on fertility, sexual function, and the exciting world of ongoing research and future developments, all explained in simple and unique language.
- Fertility Implications
When it comes to starting a family, the seminal vesicles are more important than you might think. They’re like the behind-the-scenes crew that ensures everything runs smoothly. Here’s how:
The seminal vesicles produce a special fluid that mixes with sperm to create semen. This fluid provides vital nutrients, energy, and protection for the sperm as they embark on their journey to meet an egg. Without this nutrient-rich cocktail, the sperm would be like lost travelers without a map or supplies.
So, if the seminal vesicles aren’t working correctly, it can have a direct impact on a man’s fertility. Conditions like infections or blockages in these pouches can hinder the production and delivery of this essential fluid, making it harder for sperm to reach their destination and fertilize an egg.
In essence, the seminal vesicles are the unsung heroes of fertility, ensuring that sperm are well-equipped for their epic quest.
- Impact on Sexual Function
But the seminal vesicles aren’t just about making babies; they also have a significant role in sexual function. Think of them as the stage crew that sets the scene for an unforgettable performance.
The seminal vesicles’ contribution to semen isn’t just for show. The fluid they produce helps to lubricate and nourish the sperm, making sexual intercourse more comfortable and enjoyable for both partners. It’s like having a smooth, well-lubricated road for the sperm to travel on.
So, when the seminal vesicles are functioning correctly, it can enhance sexual pleasure and overall sexual function. On the flip side, issues with these pouches can lead to discomfort or pain during ejaculation, which can impact sexual satisfaction.
- Research and Future Developments
The world of medicine is always evolving, and that includes our understanding of the seminal vesicles and their role in reproductive health. Researchers are continually exploring new avenues to improve our knowledge and treatments related to these tiny organs.
Some ongoing areas of research include:
Advanced Imaging: Scientists are developing more precise and non-invasive imaging techniques to better understand the structure and function of the seminal vesicles.
Treatment Innovations: Medical professionals are exploring new therapies and treatments for conditions affecting the seminal vesicle, aiming for more effective and less invasive options.
Reproductive Medicine: Researchers are delving into assisted reproductive technologies that can help individuals or couples overcome fertility challenges related to seminal vesicle issues.
In conclusion, the seminal vesicles are more than just small pouches in the male reproductive system; they are integral to fertility, sexual function, and overall reproductive health. Understanding their importance can shed light on the complexities of human reproduction. And with ongoing research and advancements in medical science, the future looks promising for improving the understanding and treatment of seminal vesicle-related issues.
Conclusion
In conclusion, our journey through the world of the seminal vesicle has revealed its remarkable significance in the male reproductive system and overall health. These unassuming pouches, tucked away behind the scenes, play pivotal roles in fertility, sexual function, and the creation of life itself.
From their formation during fetal development to their transformation during puberty, the seminal vesicles silently prepare for their essential duties. They produce the nutrient-rich fluid that nourishes and supports sperm on their quest to fertilize an egg, ensuring the continuation of the human species.
However, like any part of the body, the seminal vesicles can face challenges. Conditions such as seminal vesiculitis, cysts, or even the rare occurrence of cancer can disrupt their function. Fortunately, with modern medicine’s arsenal of antibiotics, surgical procedures, and pain management techniques, many of these issues can be diagnosed and treated effectively.
Additionally, we’ve learned how advancements in imaging technologies and ongoing research are paving the way for a deeper understanding of the seminal vesicles and more innovative treatments.
So, as we wrap up this exploration, remember the unsung heroes of the reproductive system—the seminal vesicles. Their vital role in fertility and sexual function reminds us of the intricate design of the human body and the ongoing efforts of scientists and healthcare professionals to ensure our reproductive health and overall well-being.
As our understanding of the seminal vesicles continues to evolve, so does our ability to support and enhance human fertility and sexual satisfaction, offering hope for the future of reproductive health.